

Subsequently, rsbA facilitated biofilm and extracellular polysaccharide formation.
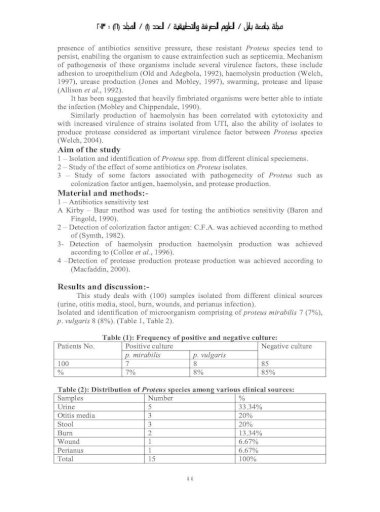
This gene regulates the swarming manner, which encodes a sensory and act as a protein sensor of environmental circumstances. The rsbA gene expresses a histidine-containing phosphotransmitter of the bacterial two-component signaling system. The luxS gene produces signal that is used to sense the interaction of species and its cell density in a polymicrobial community that plays critical roles in the virulence genes regulation. Another group of virulence genes is the quorum sensing ( luxS, and rsbA). mirabilis facilitating the bacterial adherence and biofilm formation. The alteration of pH is important in catheter colonization of P. Urease is required for urolithiasis, where it contributes in hydrolyzing urea to release ammonia, thereby increasing urinary pH, resulting in precipitation of calcium and magnesium compounds, and urinary stone formation. This enzyme catalyzes the kidney and bladder stone formation or blocks indwelling urinary catheters. Urease ( ureC1) is a virulence gene that is important in P. mirabilis encodes many virulence genes involved in infection. Isolated Proteus mirabilis has shown multiple drug-resistance ability to the used antibiotics. The bacterium was shown to be highly sensitive to streptomycin (100%), erythromycin (85%), and sparfloxacin (75%), whereas it showed high resistance to amoxicillin (100%), tetracycline (95%), and cefuroxime (80%). mirabilis is becoming resistant to antibiotics commonly used in the treatment of UTI. mirabilis strains are responsible for the majority of complicated urinary tract infections. Bacteriuria, kidney stones, catheter obstruction, acute pyelonephritis, and fever can be developed by P. Proteus mirabilis is one of the most common Gram-negative bacteria that can cause UTIs.

mirabilis resistance to antimicrobials has been demonstrated. In conclusion, an association between the presence of urovirulence genes of P. Nitrofurantoin antimicrobial susceptibility was significantly associated with the presence each of hpmA, ureC1, rpoA, atfA, atfC, mrpA, and pm1. Ceftriaxone antimicrobial susceptibility was significantly associated with the presence each of hpmA, ureC1, rpoA, atfC, mrpA, and pm1. Sulfamethoxazole antimicrobial susceptibility was significantly associated with the presence atfA. Cephalexin antimicrobial susceptibility was significantly associated with the presence each of ureC1 and atfC. Significant associations ( ) were detected between antimicrobial susceptibility of each of the following antibiotics and the presence virulence genes. The rate of susceptibility for ceftriaxone was 96.8%, followed by norfloxacin (82.5%), gentamicin (71.4%), ciprofloxacin (69.8%), cephalexin (52.4%), nalidixic acid (42.9%), sulfamethoxazole (39.7%), ampicillin (36.5%), and nitrofurantoin (3.2%). mirabilis virulence genes were detected in more than 90% of the isolates except hlyA gene, which was detected in only 23.8% of the isolates. mirabilis, namely, hpmA, hpmB, rsbA, luxS, ureC1, hlyA, rpoA, atfA, atfC, mrpA, and pm1 were detected in the isolates via PCR detection method. mirabilis isolates were collected from urine specimens of patients suffering from UTI. mirabilis virulence genes and to characterize the antibiotic susceptibility profile of P. mirabilis strains isolated from UTI patients by the detection of several P.
The aims of the present study were to determine the prevalence of the uropathogenic P. mirabilis strains are poorly identified among UTI patients. Proteus mirabilis is the third most common bacterium that can cause complicated UTI, especially in catheterized patients.


 0 kommentar(er)
0 kommentar(er)
